The following is an excerpt from the book Biomechanics of Injury-3rd Edition (by Ronald F. Zernicke, Steven Broglio & William C. Whiting) with commentary for clarity and correlation.
Of all cervical disorders, whiplash-related injuries are among the most common and most misunderstood, because the term is used to describe both an injury mechanism (i.e., cervical acceleration–deceleration) and a clinical syndrome.
Whiplash can occur from a fall, a hit on the head, a push from behind or a mild car accident.
Whiplash mechanics are complex and not well understood, but the Quebec Task Force on Whiplash-Associated Disorders defined whiplash as “an acceleration–deceleration mechanism of energy transfer to the neck which may result from rear-end or side impact, predominately in motor vehicle accidents, and from other mishaps. The energy transfer may result in bony or soft tissue injuries (whiplash injury), which may in turn lead to a wide variety of clinical manifestations (whiplash-associated disorders)” (Cassidy et al. 1995, p. 22).
The injury that causes whiplash can injure the neck and the brain.
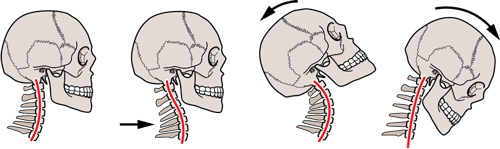
In recent decades many studies have been conducted to determine the mechanisms of whiplash, which is typically characterized as involving a hyperextension mechanism. Using a motor vehicle crash as an example, the vehicle is violently pushed forward, accelerating the occupant’s trunk and shoulders anteriorly. The head remains stable (based on Newton’s first law), effectively forcing the neck into hyperextension. Once its inertia is overcome, the head is thrown (whiplashed) forward into flexion.
Modern research efforts have shown the hyperextension model to be too simplistic, inadequately describing the complex motion of the cervical spine during whiplash. “The critical revision brought about by modern research into whiplash is that it is not a cantilever movement that is injurious; i.e., it is not an extension–flexion movement of the head, as was commonly believed previously. Rather, within less than 150 ms after impact, the cervical spine is compressed. During this period the cervical spine buckles; upper cervical segments are flexed while lower segments extend around abnormally located axes of rotation” (Bogduk and Yoganandan 2001, p. 272). The simultaneous upper cervical flexion and lower cervical extension results in an S-shaped neck curvature within 75 ms of impact (figure 8.17), then gives way to a C-shaped hyperextension curvature (Grauer et al.1997). These motions place both the lower cervical spine and upper cervical spine at risk of injury from the rear-impact mechanism (Panjabi, Pearson et al. 2004).
If your head and neck is turned to one side when the accident occurs the injures may be worse than if you were looking straight forward.
Although usually viewed as a sagittal plane injury caused by a rear-end impact, whiplash can also result from lateral or frontal forces with their own unique injury pattern. In addition, motion of the neck is not confined to a single plane. If a driver is looking to the side at the moment of impact, for example, the injury mechanism involves a combination of hyperextension and rotation. In this case the pre-impact rotation enhances the effect of the impact as the cervical structures are prestretched, which may enhance the injurious effect of the impact forces.
Car accidents commonly cause TMJ and brain related injuries. Our patients commonly have TMJ (TMD) pain relief when we rehabilitate their neck injuries from the accident.
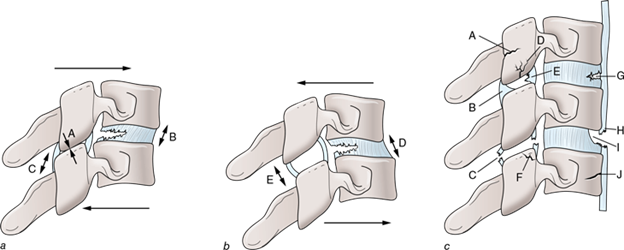
At first glance, whiplash might appear a simple injury mechanism. However, “in an individual accident there is likely to be a complex interaction between different forces depending upon the speed and direction of impact and the attitude of the head and neck” (Barnsley et al. 1994, p. 288). In addition to the cervical musculature, spinous ligaments, intervertebral discs, vertebral bodies, and facet (zygapophyseal) joints, the brain and even the temporomandibular joint can be involved (e.g., Davis 2000; Ito et al. 2004; Panjabi, Ito et al. 2004; Pearson et al. 2004). Various mechanisms and potential injury sites are shown in the figure below. Whiplash-associated disorders can manifest as both clinical and psychosocial symptoms (Eck et al. 2001). Possible symptoms are listed in table below the image.
Here's a simple way to classify the whiplash injuries from a car accident.
From the clinical perspective, whiplash is categorized into five grades (Pastakia and Kumar 2011):
o 0: No neck pain, stiffness, or physical signs
o 1: Complaints of neck pain with stiffness or tenderness but no physical signs noted - some patients
o 2: Neck pain and stiffness complaints with decreased range of motion and point tenderness - most patients
o 3: Neck pain and stiffness complaints with neurological signs - some patients
o 4: Neck pain and stiffness complaints with fracture, dislocation, or spinal cord injury - we refer to a specialist
We have been treating patients with injuries from car accidents (like whiplash) for 28 years. Check out our blog on the injuries seen on x-ray and an example of a treatment program we use. Email us at info@thcksq.com or call 610-444-8155 to speak with a doctor about your current or old injuries.